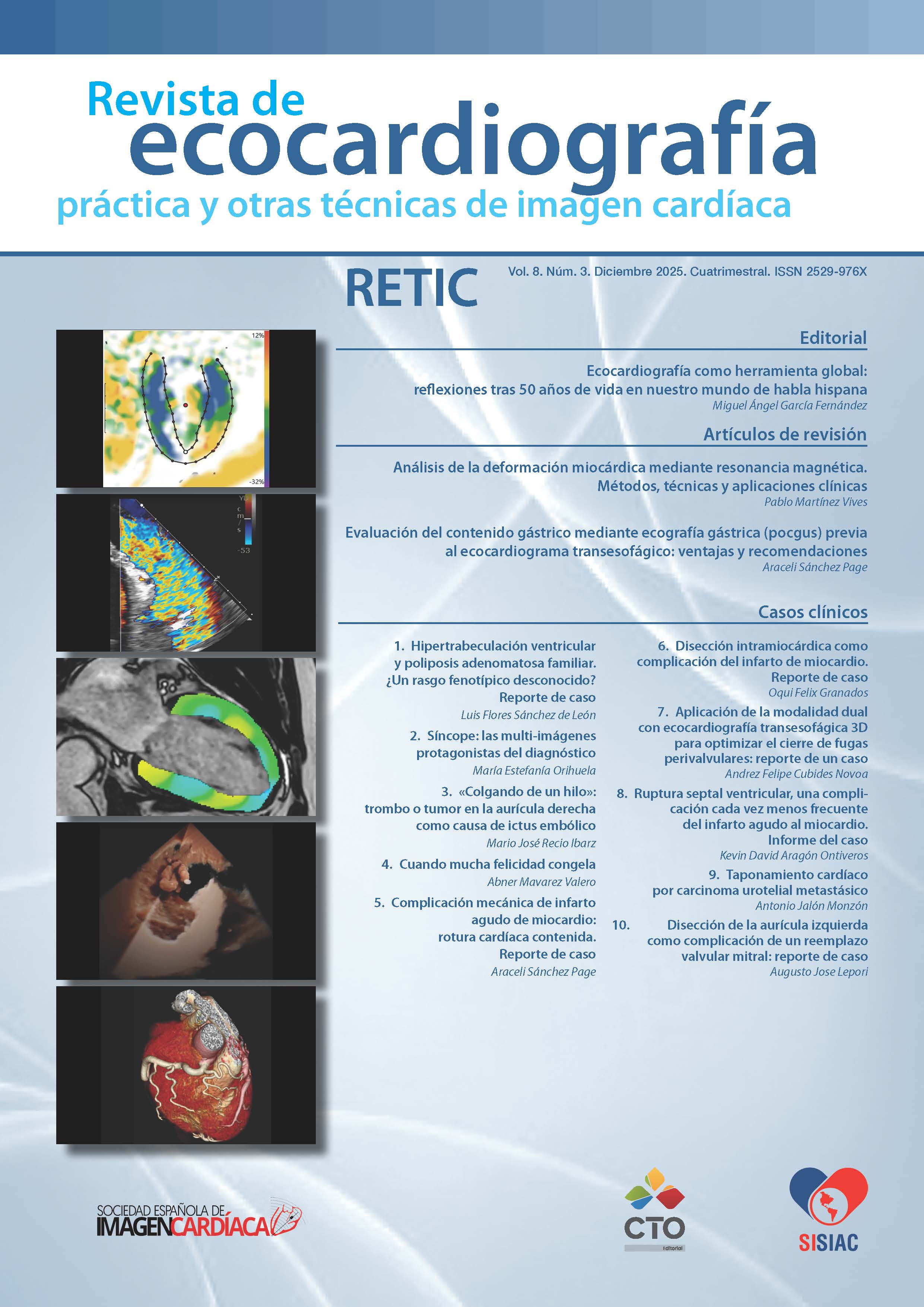
Evaluación del contenido gástrico mediante ecografía gástrica (pocgus) previa al ecocardiograma transesofágico: ventajas y recomendaciones
DOI:
https://doi.org/10.37615/retic.v8n3a3Palabras clave:
aspiración, ultrasonido gástrico en el punto de atención, ecocardiografía transesofágicaResumen
El riesgo de aspiración gástrica (inhalación de contenido oral, faríngeo o gástrico hacia las vías aéreas inferiores)
durante un procedimiento anestésico o en el periodo perioperatorio se asocia directamente con un aumento de la morbilidad y mortalidad o lesiones permanentes. La Ecocardiografía Transesofágica (ETE) podría considerarse similar a una endoscopia superior o gastroscopia con abolición de los reflejos del tracto gastrointestinal durante la sedación y el consecuente riesgo de aspiración pulmonar especialmente si experimentan factores de riesgo. En el escenario previo a la realización de la ETE en el paciente adulto, la ecografía gástrica realizada por el mismo ecocardiografista y sin cambiar el transductor ni la configuración o preset puede confirmar o descartar estómago lleno y riesgo de aspiración, por lo que este artículo es una propuesta de abordaje para reducir la aspiración durante el procedimiento y sus respectivas complicaciones.
Descargas
Métricas
Citas
Warner, Mark A., Mary Ellen Warner, and Joseph G. Weber. "Clinical significance of pulmonary aspiration during the perioperative period." Anesthesiology 78.1 (1993): 56-62. https://doi.org/10.1097/00000542-199301000-00010 DOI: https://doi.org/10.1097/00000542-199301000-00010
Lienhart, André, et al. "Preliminary results from the SFAR-iNSERM inquiry on anaesthesia-related deaths in France: mortality rates have fallen ten-fold over the past two decades." Bulletin de L'academie Nationale de Medecine 188.8 (2004): 1429-37. https://doi.org/10.1016/s0001-4079(19)33666-0 DOI: https://doi.org/10.1016/S0001-4079(19)33666-0
MENDELSON, CURTIS L. "The aspiration of stomach contents into the lungs during obstetric anesthesia." Survey of Anesthesiology 38.03 (1994): 185. https://doi.org/10.1097/00132586-199406000-00059 DOI: https://doi.org/10.1097/00132586-199406000-00059
Lienhart, Andre, et al. "Survey of anesthesia-related mortality in France." The Journal of the American Society of Anesthesiologists 105.6 (2006): 1087-1097. https://doi.org/10.1097/00000542-200612000-00008 DOI: https://doi.org/10.1097/00000542-200612000-00008
- Hahn, Rebecca T., et al. "Guidelines for performing a comprehensive transesophageal echocardiographic examination: recommendations from the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists." Journal of the American Society of Echocardiography 26.9 (2013): 921-964. https://doi.org/10.1016/j.echo.2013.07.009 DOI: https://doi.org/10.1016/j.echo.2013.07.009
-Cook, Tim, Jane Harper, and Nick Woodall. "Report of the NAP4 airway project." Journal of the Intensive Care Society 12.2 (2011): 107-111. https://doi.org/10.1177/175114371101200206 DOI: https://doi.org/10.1177/175114371101200206
- Warner, Mark A., et al. "Pulmonary aspiration of gastric contents: a closed claims analysis." Anesthesiology 135.2 (2021): 284-291.
https://doi.org/10.1097/aln.0000000000003831 DOI: https://doi.org/10.1097/ALN.0000000000003831
- Sakai, Tetsuro, et al. "The incidence and outcome of perioperative pulmonary aspiration in a university hospital: a 4-year retrospective analysis." Anesthesia & Analgesia 103.4 (2006): 941-947. https://doi.org/10.1213/01.ane.0000237296.57941.e7 DOI: https://doi.org/10.1213/01.ane.0000237296.57941.e7
- Berkmen, Yahya M. "Aspiration and inhalation pneumonias." Seminars in roentgenology. Vol. 15. No. 1. WB Saunders, 1980.
https://doi.org/10.1016/0037-198x(80)90040-1 DOI: https://doi.org/10.1016/0037-198X(80)90040-1
- Raidoo, D. M., et al. "Critical volume for pulmonary acid aspiration: reappraisal in a primate model." BJA: British Journal of Anaesthesia 65.2 (1990): 248-250. https://doi.org/10.1093/bja/65.2.248 DOI: https://doi.org/10.1093/bja/65.2.248
- Van de Putte, Peter, et al. "When fasted is not empty: a retrospective cohort study of gastric content in fasted surgical patients." BJA: British Journal of Anaesthesia 118.3 (2017): 363-371. https://doi.org/10.1093/bja/aew435 DOI: https://doi.org/10.1093/bja/aew435
- Hakak, S., C. L. McCaul, and L. Crowley. "Ultrasonographic evaluation of gastric contents in term pregnant women fasted for six hours." International Journal of Obstetric Anesthesia 34 (2018): 15-20. https://doi.org/10.1016/j.ijoa.2018.01.004 DOI: https://doi.org/10.1016/j.ijoa.2018.01.004
- Kluger, M. T., and T. G. Short. "Aspiration during anaesthesia: a review of 133 cases from the Australian Anaesthetic Incident Monitoring Study (AIMS)." Anaesthesia 54.1 (1999): 19-26. https://doi.org/10.1046/j.1365-2044.1999.00642.x DOI: https://doi.org/10.1046/j.1365-2044.1999.00642.x
- Green, S. M., K. P. Mason, and B. S. Krauss. "Pulmonary aspiration during procedural sedation: a comprehensive systematic review." BJA: British Journal of Anaesthesia 118.3 (2017): 344-354. https://doi.org/10.1093/bja/aex004 DOI: https://doi.org/10.1093/bja/aex004
- Wang, Jing, et al. "Ultrasonic assessment of gastric solid contents in patients undergoing upper endoscope with sedation." BMC anesthesiology 24.1 (2024): 317. https://doi.org/10.1186/s12871-024-02688-2 DOI: https://doi.org/10.1186/s12871-024-02688-2
- Kallmeyer, Ian J., et al. "The safety of intraoperative transesophageal echocardiography: a case series of 7200 cardiac surgical patients." Anesthesia & Analgesia 92.5 (2001): 1126-1130. https://doi.org/10.1097/00000539-200105000-00009 DOI: https://doi.org/10.1097/00000539-200105000-00009
- Practice Guidelines for Sedation and Analgesia by Non-Anesthesiologists. The Journal of the American Society of Anesthesiologists 96(4):p 1004-1017, April 1, 2002. https://doi.org/10.1097/00000542-200204000-00031 DOI: https://doi.org/10.1097/00000542-200204000-00031
- Force, ASA Task. "Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: a report by the American Society of Anesthesiologists Task Force on Preoperative Fasting." Anesthesiology 90 (1999): 896-905. https://doi.org/10.1097/00000542-199903000-00034 DOI: https://doi.org/10.1097/00000542-199903000-00034
- Tm, Cook. "Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: anaesthesia." Br J Anaesth 106 (2011): 617-631. https://doi.org/10.1093/bja/aer058 DOI: https://doi.org/10.1093/bja/aer058
- Joshi, Girish P., et al. "2023 American society of anesthesiologists practice guidelines for preoperative fasting: carbohydrate-containing clear liquids with or without protein, chewing gum, and pediatric fasting duration—a modular update of the 2017 American society of anesthesiologists practice guidelines for preoperative fasting." Anesthesiology 138.2 (2023): 132-151.
https://doi.org/10.1097/aln.0000000000004381 DOI: https://doi.org/10.1097/ALN.0000000000004381
-Practice Guidelines for Preoperative Fasting and the Use of Pharmacologic Agents to Reduce the Risk of Pulmonary Aspiration: Application to Healthy Patients Undergoing Elective Procedures. An Updated Report by the American Society of Anesthesiologists Task Force on Preopera- tive Fasting and the Use of Pharmacologic Agents to Reduce the Risk of Pulmonary Aspiration. Anesthesiology. 2017;126(3):376–93.
https://doi.org/10.1097/aln.0000000000001452 DOI: https://doi.org/10.1097/ALN.0000000000001452
- American Society of Anesthesiologists Committee. "Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists Committee on Standards and Practice Parameters." Anesthesiology 114.3 (2011): 495-511. https://doi.org/10.1097/aln.0b013e3181fcbfd9 DOI: https://doi.org/10.1097/ALN.0b013e3181fcbfd9
- van Zuylen, Mark L., et al. "Perioperative management of long-acting glucagon-like peptide-1 (GLP-1) receptor agonists: concerns for delayed gastric emptying and pulmonary aspiration." British Journal of Anaesthesia 132.4 (2024): 644-648.
https://doi.org/10.1016/j.bja.2024.01.001 DOI: https://doi.org/10.1016/j.bja.2024.01.001
- Jalleh, Ryan J., et al. "Gastrointestinal effects of GLP-1 receptor agonists: mechanisms, management, and future directions." The Lancet Gastroenterology & Hepatology 9.10 (2024): 957-964. https://doi.org/10.1016/s2468-1253(24)00188-2 DOI: https://doi.org/10.1016/S2468-1253(24)00188-2
- Sen, Sudipta, et al. "Glucagon-like peptide-1 receptor agonist use and residual gastric content before anesthesia." JAMA surgery 159.6 (2024): 660-667. https://doi.org/10.1001/jamasurg.2024.0111 DOI: https://doi.org/10.1001/jamasurg.2024.0111
- McIsaac, Daniel I., and Gregory L. Bryson. "Glucagon-like peptide-1 receptor agonists and aspiration risk." bmj 387 (2024).
https://doi.org/10.1136/bmj.q1986 DOI: https://doi.org/10.1136/bmj.q1986
- Marroquin‐Harris, M., and B. Olesnicky. "Aspiration risk with glucagon‐like peptide 1 (GLP‐1) agonists." Anaesthesia 78.12 (2023): 1524-1524. https://doi.org/10.1111/anae.16099 DOI: https://doi.org/10.1111/anae.16099
- Gulak, Michael A., and Patricia Murphy. "Regurgitation under anesthesia in a fasted patient prescribed semaglutide for weight loss: a case report." Canadian Journal of Anesthesia/Journal canadien d'anesthésie 70.8 (2023): 1397-1400.
https://doi.org/10.1007/s12630-023-02521-3 DOI: https://doi.org/10.1007/s12630-023-02521-3
- Fujino, Erina, et al. "Anesthesia considerations for a patient on semaglutide and delayed gastric emptying." Cureus 15.7 (2023).
https://doi.org/10.7759/cureus.42153 DOI: https://doi.org/10.7759/cureus.42153
- Sherwin, Marc, et al. "Influence of semaglutide use on the presence of residual gastric solids on gastric ultrasound: a prospective observational study in volunteers without obesity recently started on semaglutide." Canadian Journal of Anesthesia/Journal canadien d'anesthésie 70.8 (2023): 1300-1306. https://doi.org/10.1007/s12630-023-02549-5 DOI: https://doi.org/10.1007/s12630-023-02549-5
- Yeo, Yee Hui, et al. "Increased risk of aspiration pneumonia associated with endoscopic procedures among patients with glucagon-like peptide 1 receptor agonist use." Gastroenterology 167.2 (2024): 402-404. https://doi.org/10.1053/j.gastro.2024.03.015 DOI: https://doi.org/10.1053/j.gastro.2024.03.015
- Dixit, Anjali A., et al. "Preoperative GLP-1 receptor agonist use and risk of postoperative respiratory complications." Jama 331.19 (2024): 1672-1673. https://doi.org/10.1001/jama.2024.5003 DOI: https://doi.org/10.1001/jama.2024.5003
- Wu, Fei, et al. "Association of glucagon-like peptide receptor 1 agonist therapy with the presence of gastric contents in fasting patients undergoing endoscopy under anesthesia care: a historical cohort study." Canadian Journal of Anesthesia/Journal canadien d'anesthésie 71.7 (2024): 958-966. https://doi.org/10.1007/s12630-024-02719-z DOI: https://doi.org/10.1007/s12630-024-02781-7
- Camilleri, Michael. "Definite benefits of GLP-1 receptor agonists: what is the risk of gastroparesis and lung aspiration?." Gut 74.3 (2025): 342-345. https://doi.org/10.1136/gutjnl-2024-333036 DOI: https://doi.org/10.1136/gutjnl-2024-333036
- Amini, Ruaa Al Sakka, et al. "Risk of Aspiration Pneumonitis After Elective Esophagogastroduodenoscopy in Patients on Glucagon-Like Peptide-1 Receptor Agonists." Cureus 16.8 (2024). https://doi.org/10.7759/cureus.66311 DOI: https://doi.org/10.7759/cureus.66311
- Alkabbani, Wajd, et al. "Glucagon-like peptide-1 receptor agonists before upper gastrointestinal endoscopy and risk of pulmonary aspiration or discontinuation of procedure: cohort study." bmj 387 (2024). https://doi.org/10.1136/bmj-2024-080340 DOI: https://doi.org/10.1136/bmj-2024-080340
- Ushakumari, Deepu S., and Robert N. Sladen. "ASA consensus-based guidance on preoperative management of patients on glucagon-like peptide-1 receptor agonists." Anesthesiology (2023). https://doi.org/10.1097/aln.0000000000004776 DOI: https://doi.org/10.1097/ALN.0000000000004776
- Marino, E. C., et al. "Rastreio e controle da hiperglicemia no perioperatório." Diretriz Oficial da Sociedade Brasileira de Diabetes [Internet] (2023): 5238993-2023. https://doi.org/10.29327/5238993.2023-7 DOI: https://doi.org/10.29327/5238993.2023-7
- Wang, Jing, et al. "Ultrasound assessment of gastric residual volume in patients over 60 years of age undergoing gastroscopy under sedation: a prospective cohort study." Canadian Journal of Anesthesia/Journal canadien d'anesthésie 70.8 (2023): 1315-1322. https://doi.org/10.1007/s12630-023-02523-1 DOI: https://doi.org/10.1007/s12630-023-02523-1
- Arzola, Christian, et al. "Bedside Gastric Ultrasonography in Term Pregnant Women Before Elective Cesarean Delivery: A Prospective Cohort Study." Obstetric Anesthesia Digest 36.3 (2016): 146-147. https://doi.org/10.1097/01.aoa.0000489470.14780.bd
- Sabry, Rabab, et al. "Evaluation of gastric residual volume in fasting diabetic patients using gastric ultrasound." Acta Anaesthesiologica Scandinavica 63.5 (2019): 615-619. https://doi.org/10.1111/aas.13315
- Kruisselbrink, R., et al. "Ultrasound assessment of gastric volume in severely obese individuals: a validation study." BJA: British Journal of Anaesthesia 118.1 (2017): 77-82. https://doi.org/10.1093/bja/aew400
-Ohashi Y, Walker JC, Zhang F, et al. Preoperative gastric residual volumes in fasted patients measured by bedside ultrasound: a
prospective observational study. Anaesth Intensive Care 2018; 46: 608-13. https://doi.org/10.1177/0310057x1804600612 DOI: https://doi.org/10.1177/0310057X1804600612
-Bouvet L, Desgranges FP, Aubergy C, Boselli E, Dupont G, Allaouchiche B, et al. Prevalence and factors predictive of full stomach in elective and emergency surgical patients: a prospective cohort study. BJA Br J Anaesth. 2017;118(3):372–9. https://doi.org/10.1093/bja/aew462 DOI: https://doi.org/10.1093/bja/aew462
-Nimmo WS, Wilson J, Prescott LF. Narcotic analgesics and delayed gastric emptying during labour. Lancet (London, England). 1975;1(7912):890–3. https://doi.org/10.1016/s0140-6736(75)91687-6 DOI: https://doi.org/10.1016/S0140-6736(75)91687-6
-Billeaud C, Guillet J, Sandler B. Gastric emptying in infants with or without gastro-oesophageal reflux according to the type of milk. Eur J Clin Nutr. 1990;44(8):577–83. https://doi.org/10.1136/gut.47.5.661 DOI: https://doi.org/10.1136/gut.47.5.661
- Splinter, W. M., and J. D. Schaefer. "Ingestion of clear fluids is safe for adolescents up to 3 h before anaesthesia." British Journal of Anaesthesia 66.1 (1991): 48-52. https://doi.org/10.1093/bja/66.1.48 DOI: https://doi.org/10.1093/bja/66.1.48
- Maughan, R. J., and J. B. Leiper. "Methods for the assessment of gastric emptying in humans: an overview." Diabetic Medicine: a Journal of the British Diabetic Association 13.9 Suppl 5 (1996): S6-10.
- Kline, J., et al. "Accuracy in evaluating gastric ultrasound images before and after brief training." Anaesthesiology Ready to submit your research (2017).
- Ramsingh, Davinder, John Christian Fox, and William C. Wilson. "Perioperative point-of-care ultrasonography: an emerging technology to be embraced by anesthesiologists." Anesthesia & Analgesia 120.5 (2015): 990-992. https://doi.org/10.1213/ane.0000000000000702 DOI: https://doi.org/10.1213/ANE.0000000000000702
- Kendall, John L., Stephen R. Hoffenberg, and R. Stephen Smith. "History of emergency and critical care ultrasound: the evolution of a new imaging paradigm." Critical care medicine 35.5 (2007): S126-S130. https://doi.org/10.1097/01.ccm.0000260623.38982.83 DOI: https://doi.org/10.1097/01.CCM.0000260623.38982.83
- Perlas, Anahi, Cristian Arzola, and Peter Van de Putte. "Point-of-care gastric ultrasound and aspiration risk assessment: a narrative review." Canadian Journal of Anesthesia 65.4 (2018): 437-448. https://doi.org/10.1007/s12630-017-1031-9 DOI: https://doi.org/10.1007/s12630-017-1031-9
- Haskins, S. C., et al. "Gastric Ultrasound for the Regional Anesthesiologist and Pain Specialist." Obstetric Anesthesia Digest 39.3 (2019): 139-140. https://doi.org/10.1097/01.aoa.0000575168.45176.55 DOI: https://doi.org/10.1097/01.aoa.0000575168.45176.55
- Perlas, Anahi, et al. "Ultrasound assessment of gastric content and volume." The Journal of the American Society of Anesthesiologists 111.1 (2009): 82-89. https://doi.org/10.1097/aln.0b013e3181a97250 DOI: https://doi.org/10.1097/ALN.0b013e3181a97250
- Bouvet, Lionel, et al. "Could a single standardized ultrasonographic measurement of antral area be of interest for assessing gastric contents? A preliminary report." European Journal of Anaesthesiology| EJA 26.12 (2009): 1015-1019. https://doi.org/10.1097/eja.0b013e32833161fd DOI: https://doi.org/10.1097/EJA.0b013e32833161fd
- Segura-Grau, Elena, et al. "Reinforcing the valuable role of gastric ultrasound for volume and content assessment: an observational study." Brazilian Journal of Anesthesiology 72.06 (2022): 749-756. https://doi.org/10.1016/j.bjane.2021.07.008 DOI: https://doi.org/10.1016/j.bjane.2021.07.008
- Van de Putte, Peter, and Anahí Perlas. "Ultrasound assessment of gastric content and volume." British journal of anaesthesia 113.1 (2014): 12-22. https://doi.org/10.1093/bja/aeu151 DOI: https://doi.org/10.1093/bja/aeu151
- Arzola, Christian, et al. "Bedside Gastric Ultrasonography in Term Pregnant Women Before Elective Cesarean Delivery: A Prospective Cohort Study." Obstetric Anesthesia Digest 36.3 (2016): 146-147. https://doi.org/10.1097/01.aoa.0000489470.14780.bd
- Sabry, Rabab, et al. "Evaluation of gastric residual volume in fasting diabetic patients using gastric ultrasound." Acta Anaesthesiologica Scandinavica 63.5 (2019): 615-619. https://doi.org/10.1111/aas.13315 DOI: https://doi.org/10.1111/aas.13315
- Kruisselbrink, R., et al. "Ultrasound assessment of gastric volume in severely obese individuals: a validation study." BJA: British Journal of Anaesthesia 118.1 (2017): 77-82. https://doi.org/10.1093/bja/aew400 DOI: https://doi.org/10.1093/bja/aew400
- Bolondi, L. "Correlation between scintigraphic and ultrasonographic assessement of gastric emptying." Gastroenterology 90 (1986): 1349. https://doi.org/10.1016/0016-5085(95)26789-1 DOI: https://doi.org/10.1016/0016-5085(95)26789-1
- Giron Arango, Laura, and Anahi Perlas. "Gastric point-of-care ultrasound: a diagnostic tool that is coming of age?." Canadian Journal of Anesthesia/Journal canadien d'anesthésie 70.8 (2023): 1291-1294. https://doi.org/10.1007/s12630-023-02524-0 DOI: https://doi.org/10.1007/s12630-023-02524-0
- READ, MS, and RS VAUGHAN. "Allowing Pre-Operative Patients to Drink: Effects on Patient's Safety and Comfort of Unlimited Oral Water Until 2 Hours Before Anesthesia." Survey of Anesthesiology 36.3 (1992): 150. https://doi.org/10.1097/00132586-199206000-00023 DOI: https://doi.org/10.1097/00132586-199236030-00023
- Agarwal, A., P. Chari, and H. Singh. "Fluid deprivation before operation: the effect of a small drink." Anaesthesia 44.8 (1989): 632-634. https://doi.org/10.1111/j.1365-2044.1989.tb13581.x DOI: https://doi.org/10.1111/j.1365-2044.1989.tb13581.x
- Perlas, Anahi, et al. "Gastric sonography in the fasted surgical patient: a prospective descriptive study." Anesthesia & Analgesia 113.1 (2011): 93-97. https://doi.org/10.1213/ane.0b013e31821b98c0 DOI: https://doi.org/10.1213/ANE.0b013e31821b98c0
- Arzola, Christian, et al. "Bedside Gastric Ultrasonography in Term Pregnant Women Before Elective Cesarean Delivery: A Prospective Cohort Study." Obstetric Anesthesia Digest 36.3 (2016): 146-147. https://doi.org/10.1097/01.aoa.0000489470.14780.bd DOI: https://doi.org/10.1097/01.aoa.0000489470.14780.bd
- Perlas, Anahi, et al. "Validation of a mathematical model for ultrasound assessment of gastric volume by gastroscopic examination." Anesthesia & Analgesia 116.2 (2013): 357-363. https://doi.org/10.1213/ane.0b013e318274fc19
- Bouvet, Lionel, et al. "Clinical assessment of the ultrasonographic measurement of antral area for estimating preoperative gastric content and volume." The Journal of the American Society of Anesthesiologists 114.5 (2011): 1086-1092. https://doi.org/10.1097/aln.0b013e31820dee48 DOI: https://doi.org/10.1097/ALN.0b013e31820dee48
- Sharma S, Deo AS, Raman P. Effectiveness of standard fasting guidelines as assessed by gastric ultrasound examination: A clinical audit. Indian J Anaesth. 2018;62(10):747-752. https://doi.org/10.4103/ija.ija_54_18 DOI: https://doi.org/10.4103/ija.IJA_54_18
- Patil, Manjunath C., Pavan V. Dhulkhed, and B. Prajwal. "Ultrasonographic estimation of gastric volume in patients after overnight fasting and after ingestion of clear fluids two hours before surgery." Anaesthesia, Pain & Intensive Care 24.3 (2020):308-313.
https://doi.org/10.35975/apic.v24i3.1283 DOI: https://doi.org/10.35975/apic.v24i3.1283
-Srinivasareddy, Shubha. "Gastric Ultrasound for Gastric Content Evaluation." Turkish Journal of Anaesthesiology and Reanimation 51.6 (2023): 465. https://doi.org/10.4274/tjar.2023.231479 DOI: https://doi.org/10.4274/TJAR.2023.231479
- Perlas, Anahi, et al. "Validation of a mathematical model for ultrasound assessment of gastric volume by gastroscopic examination." Anesthesia & Analgesia 116.2 (2013): 357-363. https://doi.org/10.1213/ane.0b013e318274fc19 DOI: https://doi.org/10.1213/ANE.0b013e318274fc19
- Brady, Marian C., et al. "Preoperative fasting for adults to prevent perioperative complications." Cochrane database of systematic reviews 2010.5 (1996). https://doi.org/10.1002/14651858.cd004423 DOI: https://doi.org/10.1002/14651858.CD004423
- Ajuzieogu, O. V., et al. "Effect of routine preoperative fasting on residual gastric volume and acid in patients undergoing myomectomy." Nigerian journal of clinical practice 19.6 (2016): 816-820. https://doi.org/10.4103/1119-3077.180049 DOI: https://doi.org/10.4103/1119-3077.180049
- Scarr, M., et al. "Volume and acidity of residual gastric fluid after oral fluid ingestion before elective ambulatory surgery." CMAJ: Canadian Medical Association Journal 141.11 (1989): 1151.
- Borland, Lawrence M., et al. "Pulmonary aspiration in pediatric patients during general anesthesia: incidence and outcome." Journal of Clinical Anesthesia 10.2 (1998): 95-102. https://doi.org/10.1016/s0952-8180(97)00250-x DOI: https://doi.org/10.1016/S0952-8180(97)00250-X
- Gola, Wojciech, Michał Domagała, and Adam Cugowski. "Ultrasound assessment of gastric emptying and the risk of aspiration of gastric contents in the perioperative period." Anaesthesiology intensive therapy 50.4 (2018). https://doi.org/10.5603/ait.a2018.0029 DOI: https://doi.org/10.5603/AIT.a2018.0029
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2025 Juan Antonio Calderón González, José María Hernández Hernández

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-SinDerivadas 4.0.
RETIC se distribuye bajo la licencia Creative Commons Reconocimiento-NoComercial-SinDerivadas 4.0 Internacional (CC BY-NC-ND 4.0) https://creativecommons.org/licenses/by-nc-nd/4.0 que permite compartir, copiar y redistribuir el material en cualquier medio o formato, bajo los siguientes términos:
- Reconocimiento: debe otorgar el crédito correspondiente, proporcionar un enlace a la licencia e indicar si se realizaron cambios. Puede hacerlo de cualquier manera razonable, pero no de ninguna manera que sugiera que el licenciante lo respalda a usted o su uso.
- No comercial: no puede utilizar el material con fines comerciales.
- No Derivados: si remezcla, transforma o construye sobre el material, no puede distribuir el material modificado.
- Sin restricciones adicionales: no puede aplicar términos legales o medidas tecnológicas que restrinjan legalmente a otros de hacer cualquier cosa que permita la licencia.