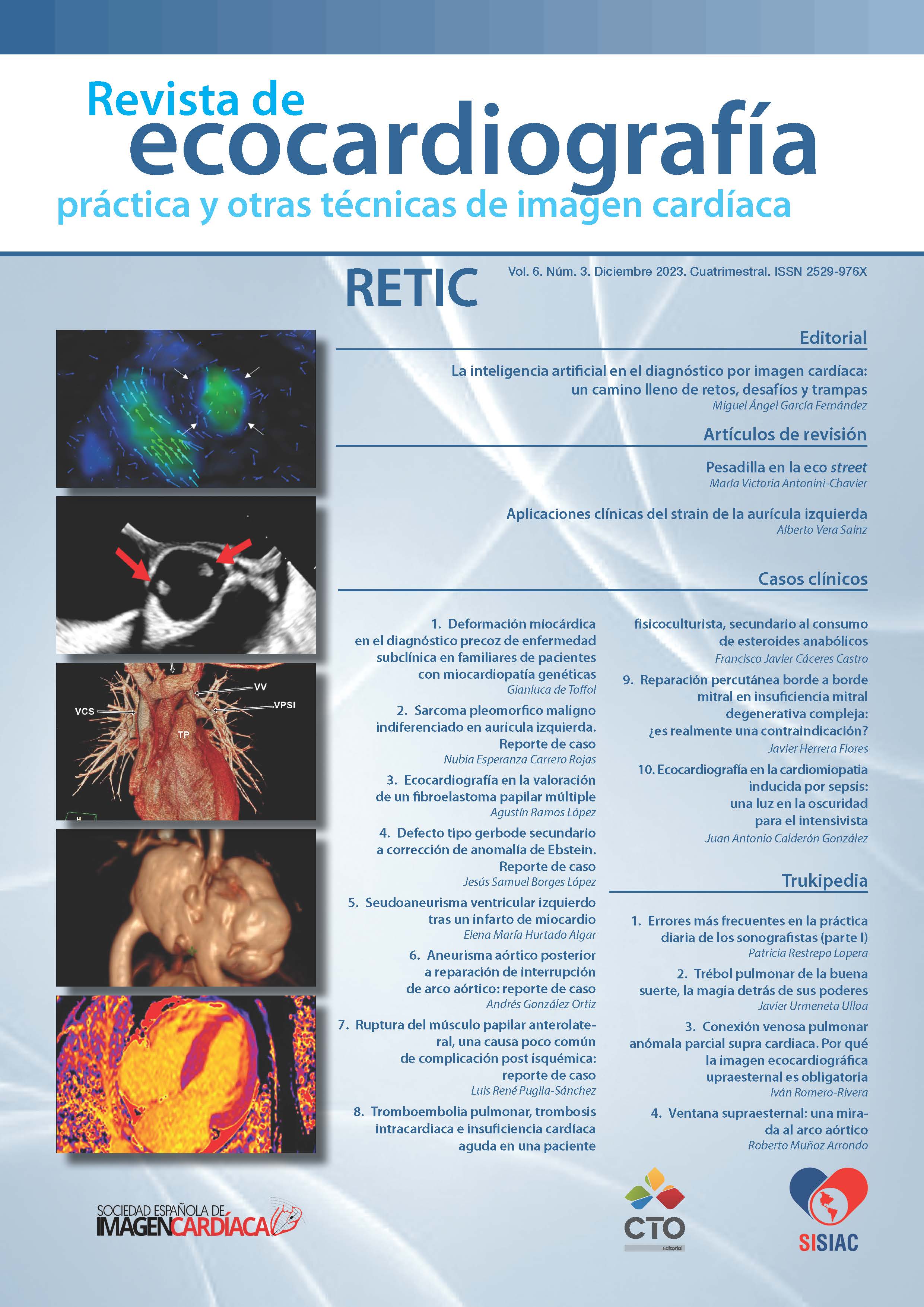
Ecocardiografía en la cardiomiopatía inducida por sepsis: una luz en la obscuridad para el intensivista.
DOI:
https://doi.org/10.37615/retic.v6n3a13Palabras clave:
cardiomiopatía por sepsis, cardiomiopatía inducida por sepsis, disfunción miocardica inducida por sepsis, ecocardiografíaResumen
Se presenta el caso de una paciente del sexo femenino de 39 años de edad la cual cursaba con estancia prolongada en un Hospital General debido a complicaciones de Cirugía abdominal. La paciente presentó deterioro súbito de la función circulatoria y requerimiento alto de fármacos vasoactivos cuya sospecha diagnóstica inicial fue Tromboembolismo pulmonar. La correcta y oportuna visualización de imágenes ecocardiográficas evitó complicaciones potencialmente letales de su tratamiento al identificar cardiomiopatia por sepsis como causa de la falla circulatoria grave.
Descargas
Métricas
Citas
Boissier F, Aissaoui N. Septic cardiomyopathy: Diagnosis and management. J Intensive Med. 2021 Dec 27;2(1):8-16. doi: https://doi.org/10.1016/j.jointm.2021.11.004 DOI: https://doi.org/10.1016/j.jointm.2021.11.004
Dalton A, Shahul S. Cardiac dysfunction in critical illness. Curr Opin Anaesthesiol. 2018 Apr;31(2):158-164. doi: https://doi.org/10.1097/ACO.0000000000000572 PMID: 29351144. DOI: https://doi.org/10.1097/ACO.0000000000000572
L’Heureux M, Sternberg M, Brath L, Turlington J, Kashiouris MG. Sepsis-Induced Cardiomyopathy: a Comprehensive Review. Curr Cardiol Rep. 2020 May 6;22(5):35. doi: https://doi.org/10.1007/s11886-020-01277-2 PMID:32377972; PMCID: PMC7222131. DOI: https://doi.org/10.1007/s11886-020-01277-2
Vallabhajosyula S, Pruthi S, Shah S, Wiley BM, Mankad SV, Jentzer JC. Basic and advanced echocardiographic evaluation of myocardial dysfunction in sepsis and septic shock. Anaesth Intensive Care. 2018 Jan;46(1):13-24. doi:https://doi.org/10.1177/0310057X1804600104 PMID: 29361252
Carbone F, Liberale L, Preda A, Schindler TH, Montecucco F. Septic Cardiomyopathy: From Pathophysiology to the Clinical Setting. Cells. 2022 Sep 11;11(18):2833. doi: https://doi.org/10.3390/cells11182833 PMID: 36139408;PMCID: PMC9496713. DOI: https://doi.org/10.3390/cells11182833
Geri G, Vignon P, Aubry A, Fedou AL, Charron C, Silva S, Repessé X, Vieillard-Baron A. Cardiovascular clusters in septic shock combining clinical and echocardiographic parameters: a post hoc analysis. Intensive Care Med. 2019 May;45(5):657-667. doi: https://doi.org/10.1007/s00134-019-05596-z Epub 2019 Mar 19. PMID: 30888443. DOI: https://doi.org/10.1007/s00134-019-05596-z
Vallabhajosyula S., Pruthi S., Shah S., Wiley B. M., Mankad S. V., Jentzer J. C. Basic and advanced echocardiographic evaluation of myocardial dysfunction in sepsis and septic shock. Anaesthesia and Intensive Care. 2019;46(1):13–24. doi: https://doi.org/10.1177/0310057x1804600104 DOI: https://doi.org/10.1177/0310057X1804600104
Orde SR, Pulido JN, Masaki M, Gillespie S, Spoon JN, Kane GC, Oh JK. Outcome prediction in sepsis: speckle tracking echocardiography based assessment of myocardial function. Crit Care. 2014 Jul 11;18(4):R149. doi: https://doi.org/10.1186/cc13987 PMID: 25015102; PMCID: PMC4227017. DOI: https://doi.org/10.1186/cc13987
Palmieri V, Innocenti F, Guzzo A, Guerrini E, Vignaroli D, Pini R. Left Ventricular Systolic Longitudinal Function as Predictor of Outcome in Patients With Sepsis. Circ Cardiovasc Imaging. 2015 Nov;8(11):e003865; discussione003865. doi: https://doi.org/10.1161/CIRCIMAGING.115.003865 PMID:26546483. DOI: https://doi.org/10.1161/CIRCIMAGING.115.003865
Ng PY, Sin WC, Ng AK, Chan WM. Speckle tracking echocardiography in patients with septic shock: a case control study (SPECKSS). Crit Care. 2016 May 14;20(1):145. doi: https://doi.org/10.1186/s13054-016-1327-0 PMID:27177587; PMCID: PMC4867983. DOI: https://doi.org/10.1186/s13054-016-1327-0
Sanfilippo F, Corredor C, Fletcher N, Landesberg G, Benedetto U, Foex P, Cecconi M. Diastolic dysfunction and mortality in septic patients: a systematic review and meta-analysis. Intensive Care Med. 2015 Jun;41(6):1004-13. doi:https://doi.org/10.1007/s00134-015-3748-7 Epub 2015 Mar 24. Erratum in:Intensive Care Med. 2015 Jun;41(6):1178-9. PMID: 25800584. DOI: https://doi.org/10.1007/s00134-015-3799-9
Pulido JN, Afessa B, Masaki M, Yuasa T, Gillespie S, Herasevich V, Brown DR, Oh JK. Clinical spectrum, frequency, and significance of myocardial dysfunction in severe sepsis and septic shock. Mayo Clin Proc. 2012 Jul;87(7):620-8. doi: https://doi.org/10.1016/j.mayocp.2012.01.018 Epub 2012 Jun 8. PMID: 22683055; PMCID: PMC3538477. DOI: https://doi.org/10.1016/j.mayocp.2012.01.018
Landesberg G, Jaffe AS, Gilon D, Levin PD, Goodman S, Abu-Baih A, Beeri R, Weissman C, Sprung CL, Landesberg A. Troponin elevation in severe sepsis and septic shock: the role of left ventricular diastolic dysfunction and right ventricular dilatation*. Crit Care Med. 2014 Apr;42(4):790-800. doi: https://doi.org/10.1097/CCM.0000000000000107 PMID: 24365861. DOI: https://doi.org/10.1097/CCM.0000000000000107
Lanspa MJ, Gutsche AR, Wilson EL, Olsen TD, Hirshberg EL, Knox DB, Brown SM, Grissom CK. Application of a simplified definition of diastolic function in severe sepsis and septic shock. Crit Care. 2016 Aug 4;20(1):243. doi: https://doi.org/10.1186/s13054-016-1421-3 PMID: 27487776; PMCID: PMC4973099. DOI: https://doi.org/10.1186/s13054-016-1421-3
Brown SM, Pittman JE, Hirshberg EL, Jones JP, Lanspa MJ, Kuttler KG, Litwin SE, Grissom CK. Diastolic dysfunction and mortality in early severe sepsis and septic shock: a prospective, observational echocardiography study. Crit Ultrasound J. 2012 May 4;4(1):8. doi: https://doi.org/10.1186/2036-7902-4-8 PMID: 22870900; PMCID: PMC3512479. DOI: https://doi.org/10.1186/2036-7902-4-8
Landesberg G, Gilon D, Meroz Y, Georgieva M, Levin PD, Goodman S, Avidan A, Beeri R, Weissman C, Jaffe AS, Sprung CL. Diastolic dysfunction and mortality in severe sepsis and septic shock. Eur Heart J. 2012 Apr;33(7):895-903. doi: https://doi.org/10.1093/eurheartj/ehr351 Epub 2011 Sep 11. PMID:21911341; PMCID: PMC3345552. DOI: https://doi.org/10.1093/eurheartj/ehr351
Rolando G, Espinoza ED, Avid E, Welsh S, Pozo JD, Vazquez AR, Arzani Y, Masevicius FD, Dubin A. Prognostic value of ventricular diastolic dysfunction in patients with severe sepsis and septic shock. Rev Bras Ter Intensiva. 2015 Oct-Dec;27(4):333-9. doi: https://doi.org/10.5935/0103-507X.20150057 PMID: 26761470; PMCID: PMC4738818. DOI: https://doi.org/10.5935/0103-507X.20150057
Monnet X, Teboul JL. Assessment of fluid responsiveness: recent advances. Curr Opin Crit Care. 2018 Jun;24(3):190-195. doi: https://doi.org/10.1097/MCC.0000000000000501 PMID: 29634494. DOI: https://doi.org/10.1097/MCC.0000000000000501
Vieillard-Baron A. Septic cardiomyopathy. Ann Intensive Care. 2011 Apr 13;1(1):6. doi: https://doi.org/10.1186/2110-5820-1-6 PMID: 21906334; PMCID:PMC3159902. DOI: https://doi.org/10.1186/2110-5820-1-6
Sato R, Nasu M. A review of sepsis-induced cardiomyopathy. J Intensive Care. 2015 Nov 11;3:48. doi: https://doi.org/10.1186/s40560-015-0112-5 PMID: 26566443; PMCID: PMC4642671. DOI: https://doi.org/10.1186/s40560-015-0112-5
McLean, A.S. Echocardiography in shock management. Crit Care 20, 275 (2016). https://doi.org/10.1186/s13054-016-1401-7 DOI: https://doi.org/10.1186/s13054-016-1401-7
Singh, K., Mayo, P. Transthoracic echocardiography and mortality in sepsis:are we there yet?. Intensive Care Med 44, 1342–1343 (2018). https://doi.org/10.1007/s00134-018-5261-2 DOI: https://doi.org/10.1007/s00134-018-5261-2
Mayo, P.H. Training in critical care echocardiography. Ann. Intensive Care 1,36 (2011). https://doi.org/10.1186/2110-5820-1-36 DOI: https://doi.org/10.1186/2110-5820-1-36
Mayo, P., Dessap, A.M. & Vieillard-Baron, A. Myths about critical care echocardiography: the ten false beliefs that intensivists should understand. Intensive Care Med 41, 1103–1106 (2015). https://doi.org/10.1007/s00134-014-3622-z DOI: https://doi.org/10.1007/s00134-014-3622-z
Expert Round Table on Echocardiography in ICU. International consensus statement on training standards for advanced critical care echocardiography. Intensive Care Med. 2014 May;40(5):654-66. doi: https://doi.org/10.1007/s00134-014-3228-5 Epub 2014 Mar 11. PMID:24615559. DOI: https://doi.org/10.1007/s00134-014-3228-5
Feng M, McSparron JI, Kien DT, Stone DJ, Roberts DH, Schwartzstein RM, Vieillard-Baron A, Celi LA. Transthoracic echocardiography and mortality in sepsis: analysis of the MIMIC-III database. Intensive Care Med. 2018 Jun;44(6):884-892. doi: https://doi.org/10.1007/s00134-018-5208-7 Epub 2018 May 28. PMID: 29806057. DOI: https://doi.org/10.1007/s00134-018-5208-7
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2023 Juan Antonio Calderón González, José María Hernández Hernández

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-SinDerivadas 4.0.
RETIC se distribuye bajo la licencia Creative Commons Reconocimiento-NoComercial-SinDerivadas 4.0 Internacional (CC BY-NC-ND 4.0) https://creativecommons.org/licenses/by-nc-nd/4.0 que permite compartir, copiar y redistribuir el material en cualquier medio o formato, bajo los siguientes términos:
- Reconocimiento: debe otorgar el crédito correspondiente, proporcionar un enlace a la licencia e indicar si se realizaron cambios. Puede hacerlo de cualquier manera razonable, pero no de ninguna manera que sugiera que el licenciante lo respalda a usted o su uso.
- No comercial: no puede utilizar el material con fines comerciales.
- No Derivados: si remezcla, transforma o construye sobre el material, no puede distribuir el material modificado.
- Sin restricciones adicionales: no puede aplicar términos legales o medidas tecnológicas que restrinjan legalmente a otros de hacer cualquier cosa que permita la licencia.