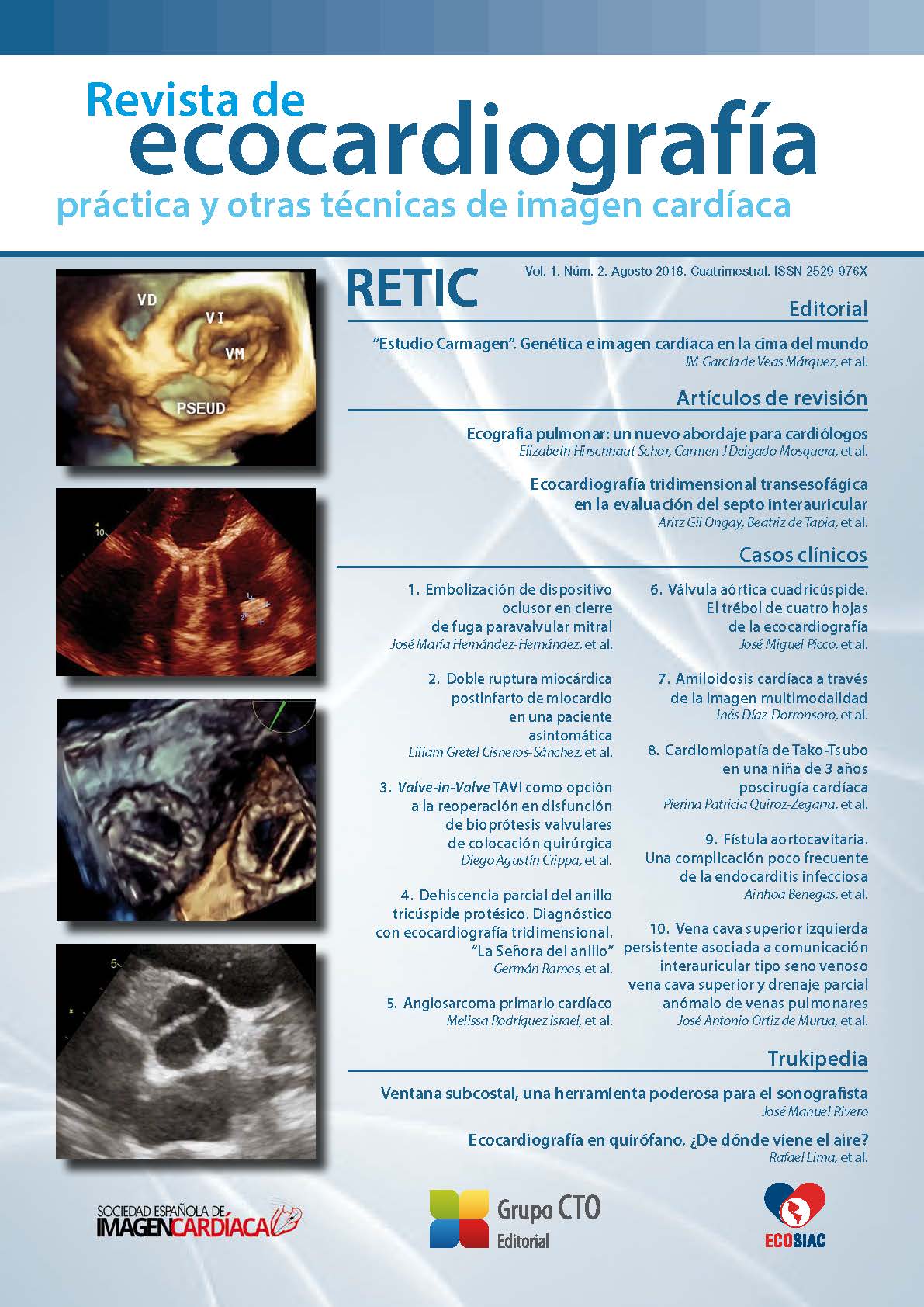
Partial dehiscence of the prosthetic tricuspid annulus. Diagnosis with three-dimensional echocardiography. "Lady of the ring".
DOI:
https://doi.org/10.37615/retic.v1n2a7Keywords:
partial dehiscence of the tricuspid prosthetic ring, tricuspid regurgitation, 3D echocardiography.Abstract
A 58-year-old woman with a history of mechanic mitral prosthesis and tricuspid prosthetic ring annuloplasty presented functional impairment and lower limbs edema. A transthoracic echocardiogram showed dilatation of right ventricle with preserved systolic function and severe eccentric tricuspid regurgitation with an unclear mechanism. Transesophageal echocardiogram revealed a partial dehiscence of the prosthetic ring. Three-dimensional (3D) “in face” reconstruction of tricuspid valve allowed an exact characterization of the defect and the design of adequate surgical strategy.
There is increasing evidence of significant postoperative residual tricuspid regurgitation. Some reports have mentioned dehiscence of the prosthetic ring as an infrequent mechanism that eventually could requires reoperation. For this reason, its diagnosis is relevant, and novel techniques such as three-dimensional echocardiography can significantly help in the decision-making process.
Downloads
Metrics
References
Rodés-Cabau J, Taramasso M, O’Gara PT. Diagnosis and treatment of tricuspid valve disease: current and future perspectives. Lancet 2016; 388: 2431- 2442. DOI: https://doi.org/10.1016/S0140-6736(16)00740-6
Wang N, Phan S, Tian DH, Yan TD, Phan K. Flexible band versus rigid ring annuloplasty for tricuspid regurgitation: a systematic review and meta-analysis. Ann Cardiothorac Surg 2017; 6 (3): 194-203. DOI: https://doi.org/10.21037/acs.2017.05.05
Parolari A, Barili F, Pilozzi A, Pacini D. Ring or suture annuloplasty for tricuspid regurgitation? A meta-analysis review. Ann Thorac Surg 2014; 98: 2255-2263. DOI: https://doi.org/10.1016/j.athoracsur.2014.06.100
Pfannmüller B, Doenst T, Eberhardt K, et al. Increased risk of dehiscence after tricuspid valve repair with rigid annuloplasty rings. J Thorac Cardiovasc Surg 2012; 143 (5): 1050-1055. DOI: https://doi.org/10.1016/j.jtcvs.2011.06.019
Tei C, Pilgrim JP, Shah PM, et al. The tricuspid valve annulus: study of size and motion in normal subjects and in patients with tricuspid regurgitation. Circulation 1982; 66: 665-671. DOI: https://doi.org/10.1161/01.CIR.66.3.665
Ton-Nu TT, Levine RA, Handschumacher MD, et al. Geometric determinants of functional tricuspid regurgitation: insights from 3-dimensional echocardiography. Circulation 2006; 114: 143-149. DOI: https://doi.org/10.1161/CIRCULATIONAHA.106.611889
Paul DM, Naran A, Pierce EL, et al. Suture dehiscence in the Tricuspid Annulus: An Ex Vivo Analysis of Tissue Strength and Composition. Ann Thorac Surg 2017; 104 (3): 820-826. DOI: https://doi.org/10.1016/j.athoracsur.2017.02.040
Pfannmuller B, Davierwala P, Misfeld M, et al. Postoperative outcome of isolated tricuspid valve operation using arrested-heart or beating heart technique. Ann Thorac Surg 2012; 94: 1218-1222. DOI: https://doi.org/10.1016/j.athoracsur.2012.05.020
Miglioranza MH, Mihaila S, Muraru D, et al. Dynamic changes in tricuspid annular diameter measurement in relation to the echocardiographic view and timing during the cardiac cycle. J Am Soc Echocardiogr 2015; 28: 226- 235. DOI: https://doi.org/10.1016/j.echo.2014.09.017
Shiota T. Role of modern 3D echocardiography in valvular heart disease. Korean J Intern Med 2014; 29 (6): 685-702. DOI: https://doi.org/10.3904/kjim.2014.29.6.685
Naqvi TZ, Rafie R, Ghalichi M. Real-time 3D TEE for the diagnosis of rightsided endocarditis in patients with prosthetic devices. JACC Cardiovasc Imaging 2010; 3 (3): 325-327. DOI: https://doi.org/10.1016/j.jcmg.2009.11.011
Sugeng L, Shernan SK, Weinert L, et al. Real-time three-dimensional transesophageal echocardiography in valve disease: comparisonwith surgical findings and evaluation of prosthetic valves. J Am Soc Echocardiog 2008; 21 (12): 1347-1354. DOI: https://doi.org/10.1016/j.echo.2008.09.006
Urmeneta Ulloa J, Molina Borao I, Aured Guallar C, et al. Three-Dimensional Echocardiography in the Evaluation of the Dehiscence of Mitral Valve Annuloplasty Ring. Circulation 2015; 132 (25): e388-390. DOI: https://doi.org/10.1161/CIRCULATIONAHA.115.016064
Begüm Uygur, Mehmet Ertürk, Hale Ünal Aksu, Aydın Yıldırım. Partial detachment of tricuspid valve annuloplasty ring detected by three-dimensional transesophageal Echocardiography. Anatol J Cardiol 2016; 7118: E 9. DOI: https://doi.org/10.14744/AnatolJCardiol.2016.7118
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2018 Germán Ramos, Mario Zapata, Manuel Rodríguez, Sebastián Herrera

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
RETIC is distributed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) license https://creativecommons.org/licenses/by-nc-nd/4.0 which allows sharing, copying and redistribution of the material in any medium or format, under the following terms:
- Attribution: you must give appropriate credit, provide a link to the license, and indicate if changes were made. You may do so in any reasonable manner, but not in any way that suggests that the licensor endorses you or your use.
- Non-commercial: you may not use the material for commercial purposes.
- No Derivatives: if you remix, transform or build upon the material, you may not distribute the modified material.
- No Additional Restrictions: you may not apply legal terms or technological measures that legally restrict others from doing anything permitted by the license.